
Breast Biopsy Guidance System Provides Superior Imaging
Women's Imaging has expanded its breast biopsy technology with a system that helps radiologists pinpoint subtle lesions and faint calcifications.
Breast cancer is the second most common cancer among U.S. women, and early detection offers a better chance of survival. October is Breast Cancer Awareness Month, making this annual campaign a good reminder to consider your breast health and to schedule your mammogram screening.
About 287,850 women in the U.S. will learn they have invasive breast cancer this year, along with 51,400 with noninvasive breast cancer. These numbers are huge. Fortunately, breast cancer rates have gone down since the 1980s. Yet, 43,250 women in the U.S. are expected to unfortunately die from this disease in 2022.
Risk Factors
Many risk factors for breast cancer are beyond your control:
- Age: Second biggest risk factor
- Family history: If a first-degree relative – mother, daughter or sister – had breast cancer or multiple relatives had breast or ovarian cancer
- Personal history: If previously diagnosed with breast cancer
- Breast density: Increases cancer risk by 1%-2%
- BRCA genes: 5%-10% of breast cancers are linked to gene mutations inherited from a mother or father.
You can, however, control these risk factors:
-
- Weight: Obesity increases risk, especially in postmenopausal women. The reason is because your body’s source of estrogen after menopause is usually fat tissue. Having more fat tissue means you have higher estrogen levels. Keep your body weight in a healthy range for your height and frame.
- Diet: A low-fat diet may reduce your risk of breast cancer. The bottom line is controlling your weight and your fat levels is important. This is not only related to breast cancer risk, but it also is important for your general health.
- Exercise: Engage in 45-60 minutes of physical exercise five or more days a week. Even getting moving and walking are the easy ways to exercise.
- Alcohol: Alcohol can limit your liver’s ability to control blood levels of the hormone estrogen, which can increase your risk.
- Smoking: Women who smoke or are former smokers are more likely to get breast cancer than nonsmokers.
Getting a Mammogram
I know many women feel they have to psych themselves up to get their mammograms. We understand, and we try to make the process as easy for you as we can.
A mammogram is an X-ray of the breast. Mammograms check breast cancer in women who have no signs or symptoms of the disease. This is what makes it a screening mammogram. We’re looking to see if you have disease.
Screening Mammogram
A screening mammogram usually involves two X-ray pictures, or images, of each breast, which makes it possible to detect tumors that cannot be felt. By the time you can feel a tumor, it’s divided millions and millions of times. We want to catch these cancers as early as possible. Microcalcifications – tiny deposits of calcium – sometimes indicate the presence of breast cancer.
Diagnostic Mammogram
Another type of mammogram is a diagnostic mammogram. This checks for breast cancer after a lump has been found. Besides a lump, signs of breast cancer can include breast pain, thickening of the skin, nipple discharge or a change in breast size or shape. A diagnostic mammogram helps us evaluate changes found during a screening mammogram and is helpful when it is difficult to obtain a screening mammogram, such as during the presence of breast implants.
3-D Versus 2-D Mammograms
A 3-D mammogram takes several images of the entire breast. A 2-D mammogram produces one image of overlapping tissue, making it somewhat difficult to detect cancers. 3-D compared to 2-D mammograms provide:
- Increased detection of invasive breast cancers
- Reduced false-positive rates, which are people who we think have cancer, but they really don’t
- Decreased callbacks for diagnostic mammograms and sonograms, which reduces patient anxiety
- Earlier detection of small breast cancers
- Greater accuracy in pinpointing the size, shape and location of abnormalities
- Fewer unnecessary biopsies or additional tests
- Greater likelihood of detecting multiple breast tumors
Breast Density
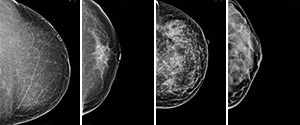
Left-right, a progression of more and more breast density.
Another issue we face is breast density, which is an uncontrollable factor you are born with. We grade these densities 1, 2, 3 and 4, with 1 being the least dense and 4 being the most (see graphic). Only about 10% of women have category 1 dense breast. A 3-D mammogram is much better than 2-D for cancer detection in women with breasts that fall into categories 2, 3 or 4.
Automated Breast Ultrasound (ABUS)
ABUS is a further way to examine significantly dense breasts. When used with a 3-D mammogram, ABUS can increase detection rates in dense breasts. ABUS uses sound waves to generate pictures, so there is no radiation.
Schedule Your Mammogram
Annual screening mammograms can catch cancer early, before you even have symptoms and when it is most treatable. Women should begin annual breast cancer screenings at age 40. Women with a family history of breast cancer should begin yearly mammograms 10 years earlier than the age of the diagnosed family member or at age 40, whichever comes first.
We provide full-service, state-of-the-art diagnosis and treatment at our Women’s Imaging Center at NKCH and at Medical Imaging at the North Oak Medical Park. We are recognized by the American College of Radiology as a Breast Imaging Center of Excellence.
NKCH Women’s Imaging Center
2790 Clay Edwards Dr.
North Kansas City, MO 64116
Monday-Friday, 6:30 a.m.-4 p.m.
Walk-in option: Monday-Friday, 7:30 a.m.-3 p.m.
Medical Imaging at North Oak Medical Park
9501 N. Oak Trafficway
Kansas City, MO 64155-2256
Monday, Tuesday and Wednesday, 7:30 a.m.- 3 p.m.
Thursday and Friday: 7:30 a.m.-4 p.m.
Same-day results accessible through myhealth, your patient portal.
Watch Dr. Formen's Lunch & Learn: Mind Over Mammogram
Explore More
A Pattern for Living
Make Your Mammogram a Must
Surviving and Thriving



