Foods That Can Fool With Your Meds
July 7, 2021By: Chelsea Stallings (left) and Megan Hickey (right)
Categories: Live Healthy, Nutrition, Prevention, Your Wellness

More often than not, the label on your over-the-counter or prescription medicine bottle reads “Take With Food.” Most people know to be aware of mixing medications, but certain foods — and some drinks — can also affect how medicine works in your body. Two North Kansas City Hospital pharmacists share their expertise.
Aged cheese, malt beer, red wine and smoked fish. If you take an MAO inhibitor, such as phenelzine (Nardil®) or selegiline (Emsam®), these foods can make your blood pressure soar.
Alcohol. As a general rule, it’s not a good idea to mix alcohol with any medication. “Alcohol should be especially avoided if you are taking the antibiotic metronidazole, or Flagyl®,” advised NKCH Pharmacist Chelsea Stallings, PharmD. “It can cause nausea and vomiting.”
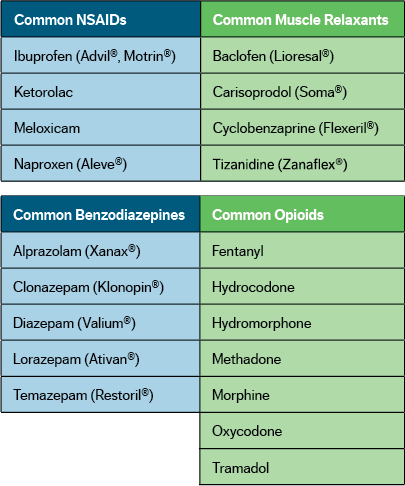
Mixing alcohol with common over-the-counter pain relievers such as nonsteroidal anti-inflammatory drugs, better known as NSAIDs, and acetaminophen, can increase your risk of serious health problems. “NSAIDs can cause gastrointestinal bleeding,” cautioned Megan Hickey, PharmD. “Mixing alcohol with Tylenol® can increase your risk of liver damage. Lastly, drinking alcohol while taking benzodiazepines, opioids or muscle relaxants can cause increased sleepiness.”
Coffee and other caffeine containing foods. Many of us love our morning cup of Joe. But, it can increase the effects of aspirin, medicines for COPD and other respiratory conditions (theophylline), antipsychotic medications (clozapine), common cold medicines with pseudoephedrine, and inhalers, such as albuterol.
“Foods and drinks with caffeine can counteract the effects of sleep aids like zolpidem (Ambien®) but boost the effects of stimulants such as methylphenidate (Ritalin®) or Adderall®,” Stallings said.
Grapefruit. This popular morning breakfast item can alter the effects of cholesterol-lowering medicines called statins. The most common statins are atorvastatin (Lipitor®), simvastatin (Zocor®), pravastatin (Pravachol®) and rosuvastatin (Crestor®).
Leafy Greens. Broccoli, kale, spinach and other vitamin K-packed foods are great for building strong bones and helping blood clot. But too much vitamin K can reduce the effects of warfarin, putting you at a higher risk for blood clots. Don’t stop eating your greens, but try to stay consistent on how much you eat each day.
Milk, cheese, yogurt and other calcium-containing foods. The calcium you get from eating dairy does a body good unless you’re on an antibiotic such as ciprofloxacin, levofloxacin, doxycycline or tetracycline. Calcium prevents your body from absorbing these medications. “It is a good rule of thumb to avoid eating foods with calcium at least two hours before and after taking these medications,” Hickey said.
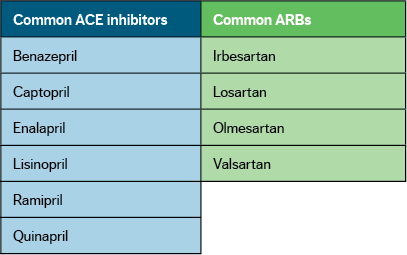
Salt substitutes. Some people may take salt substitutes to reduce their sodium intake. However, salt substitutes contain potassium. Medications like angiotensin-converting enzyme inhibitors, angiotensin receptor blockers and spironolactone can increase the amount of potassium in the body. Taking these medicines and using a salt substitute can lead to heart arrhythmias.
"Take on an Empty Stomach"
“Some medications need to be taken on an empty stomach to make sure they are absorbed properly,” Stallings said. “Typical instructions are to take these medicines at least one hour before or four hours after eating.” Common medications that require an empty stomach are levothyroxine (Synthroid®,) oral semaglutide (Rybelsus®) and alendronate (Fosamax®).
“Before starting any new medication, talk with your doctor or pharmacist about it,” Hickey added. “Make sure you understand — and follow — all instructions, including which foods are off limits.”
If you don’t have a primary care doctor, we can help.