Codfish Skin Helps Heal Wounds, Reduces Pain Levels
July 13, 2017By: Amy Bennett
Categories: High Tech

An innovative wound treatment using fish skin is bringing dramatic healing, reduction in pain and cost savings to patients at NKCH.
Vascular Surgeon Karl Stark, MD, with Midwest Aortic and Vascular Institute and director of the hospital’s Wound Healing Center, along with his colleagues, are the Northland’s only physicians using codfish skin to treat chronic wounds, including foot and leg wounds caused by diabetes.
Natural Healer
Thanks to naturally occurring and beneficial alpha omega fatty acids, the fish skin works like a scaffold. When grafted onto damaged human tissue, the material vascularizes and recreates a patient’s own cells, ultimately reducing inflammation and converting into living tissue. The U.S. Food and Drug Administration approved the product in 2013.
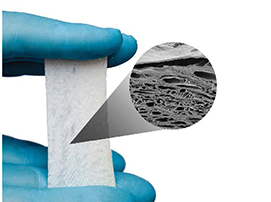
This microscopic image shows the highly porous nature of the fish skin. The fish originates off the northwest coast of Iceland in the pristine waters of the North Atlantic Ocean.
“The fish skin has no risk of disease transmission, so the manufacturer doesn’t have to prepare it in the same way it would tissue from mammals,” Dr. Stark said. “That allows the tissue to be more normal in structure and integrate better into human tissue, causing the cells to advance quickly.” The alpha omega fatty acids also work as an anti-inflammatory agent to improve pain levels.
Early in his career, Dr. Stark was drawn to patients who needed wound care. “It was sort of natural for me,” he said. “I saw how much I could improve lives by taking good care of wounds. There is a huge level of satisfaction in the physician-patient relationship of wound care because it’s hands on, and patients are so appreciative.”
Treatment
Patients typically undergo weekly outpatient fish skin applications as part of their wound care management. Dr. Stark has seen dramatic wound healing, including in patients who have diabetes and are on dialysis. Wounds for these types of patients are some of the most challenging to close. “We expect less than 10% of these wounds to ever close, but we have had some close. That is impressive, and these patients get a new lease on life,” he said.
The fish skin is 1 mm thick and can be used on large – 10-15 cm – wounds, that are too large for treatment with bovine and porcine products because of cost.
“The fish skin has no risk of disease transmission, so the manufacturer doesn’t have to prepare it in the same way it would mammalian tissue. That allows the tissue to be more normal in structure and to integrate better into human tissue.” – Karl R. Stark, MD, FACS
Insurance Coverage
Dr. Stark said insurance companies cover patients who undergo fish skin applications. If an insurance company is unfamiliar with the product, his clinic makes them aware of its applications and cost-savings.
“We don’t use fish skin unless the patient’s insurance company covers the treatment,” he said. “It’s cost-efficient, which is a big benefit.”




