At just over 1 year old, Gracelyn Eichhorn is the picture of health. Her cheerful, outgoing disposition captures the hearts of all who meet her. Gracelyn’s mom and dad, Vallri and Ryan, are grateful Gracelyn’s premature birth at 30 weeks, 1 day, and stay of 38 days was at North Kansas City Hospital’s Neonatal Intensive Care Unit.
At just over 1 year old, Gracelyn Eichhorn is the picture of health. Her cheerful, outgoing disposition captures the hearts of all who meet her. Gracelyn’s mom and dad, Vallri and Ryan, are grateful Gracelyn’s premature birth at 30 weeks, 1 day, and stay of 38 days was at North Kansas City Hospital’s Neonatal Intensive Care Unit.
Vallri’s due date was April 9, but on Jan. 27, 2021, she was transferred from an area hospital to NKCH’s Labor and Delivery unit. The only Level III NICU in the Northland and the closest for Vallri’s emergent needs, our specially trained perinatology staff care for babies born as early as 28 weeks (full term is 40 weeks) or who need intensive care.
Hand in Hand
NKCH provides this high level of care through a collaboration with Children’s Mercy Kansas City. This means their neonatologists are on the NICU every day, and neonatal nurse practitioners are on-site 24/7.
For NKCH Neonatology Chief Steven Olsen, MD, NKCH nursing, pharmacy, respiratory, radiology, obstetrical physicians and Children’s Mercy Kansas City neonatologists and nurse practitioners have made the collaboration successful.
In Vallri's Own Words
"I remember crying, thinking it was too early and too much risk."
Vallri shares the inspirational story of how the NICU saved her baby, Gracelyn.
“With additional experience and support, we lowered the gestational age from 32 weeks to 28 weeks, allowing us to take care of more mothers and their premature babies than ever before,” said Dr. Olsen, adding NKCH’s NICU also takes transfers from Missouri hospitals when Children’s Mercy Kansas City is full.
Forks in the Road
Vallri, 41, knew her age could delay conception, and, after trying naturally, she and Ryan, sought in vitro fertilization, which brought two viable embryos in January 2020. After a delay due to COVID restrictions, Vallri underwent uterine polyp removal surgery in May and then a successful frozen embryo transfer in July.
Although her first trimester went smoothly, she began experiencing extremely high blood pressures and excessive swelling by the end of her second trimester. On Jan. 27, 2021, Vallri sat at a Walmart blood pressure machine while running errands. “The top number was 170, and the bottom was around 115,” Vallri exclaimed.
After a call to her OB’s office, Vallri and Ryan drove to her birth hospital, where she was diagnosed with preeclampsia. This can lead to a hemorrhagic stroke, which is when a blood vessel breaks and bleeds into the brain, and seizures if Vallri progressed to eclampsia. She was put on a magnesium sulfate drip to help reduce her blood pressure and received steroids to speed development of her baby’s lungs.


Path to Perseverance
Vallri moved by ambulance to NKCH, where she went on bedrest in the Labor and Delivery unit. She initially responded to blood pressure medications, allowing for another round of steroids for her baby’s lung development.
Three days later, Vallri’s morning blood pressure rose to 192/116, but maximum doses of blood pressure medications were to no avail. “We weigh the risks of prematurity versus maternal health. If we can stabilize the mom, then we can try to get extra days,” said Dawn Heizman, MD, obstetrician and gynecologist with Meritas Health Pavilion for Women. “Every day matters at this gestational age, but Vallri’s health was at risk. We had to deliver.”
Vallri and her husband understood the urgency. “I remember crying, thinking it was too early and too much risk, but I trusted in everyone because I knew we were where we were supposed to be,” Vallri said.
Born Jan. 30, 2021, at 10:23 a.m. and weighing 3 pounds, Gracelyn was put on a ventilator for respiratory support. On Feb. 5, she moved to supplemental oxygen and was off all oxygen on Feb. 22.
During this time, she also went from tube feedings to Vallri’s breastmilk via bottle feedings. Because Vallri was discharged after a 10-day hospitalization, she and Ryan visited Gracelyn day and night. “The staff was amazing,” Vallri said. “They would tell us about Gracelyn’s days, and they even dressed her in clothes we provided for photos.”
On March 10, Gracelyn, who was 5 pounds, went home. “Gracelyn is spunky, outgoing and quick to make friends,” Vallri said. “She is thriving, and we cannot say enough good things about North Kansas City Hospital’s NICU.”
Explore More
Learn more about the level III Neonatal Intensive Care Unit at North Kansas City Hospital.
Related Articles

March 9, 2020
3 Sneaky IBS Triggers
For people with irritable bowel syndrome, spring may spark a flare-up in symptoms

May 31, 2024
5 Nutrition Tips for a Healthier Lifestyle
Healthy eating and proper nutrition play a big part in maintaining good health. Here's how to improve your nutrition habits.
July 8, 2021
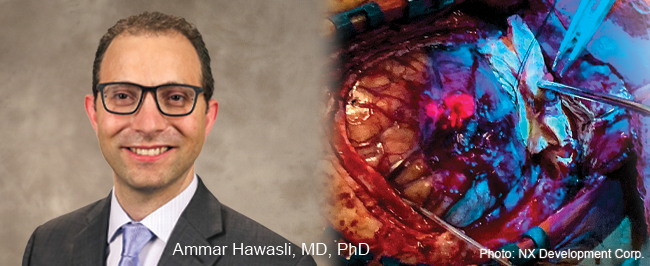
5-ALA Fluorescence Guides Neurosurgeons for More Complete Resections
Neurosurgeons Ammar Hawasli, MD, PhD, and Stephen Reintjes Jr., MD, with Meritas Health Neurosurgery, are now using a progressive treatment that allows for the more precise removal of malignant gliomas and glioblastomas.