Every year, Northland resident John Williams and his wife Vicki Young pack their bags and head to ski country for the annual Black Summit of the National Brotherhood of Skiers, the largest African American ski and snowboard association in the world. This year’s event, held in Sun Valley, ID, the first week of March 2020, drew nearly 700 members.
At the time, COVID-19 was just starting to make its presence known in the U.S. By the time John, Vicki and other NBS skiers arrived in Idaho, the virus had already settled into Sun Valley. But, no one knew it.
A week after returning from their trip, John and Vicki developed high fevers and weren’t feeling well. “We just kept getting worse,” Vicki recalled. She called their primary care provider, who asked them to come to the clinic.
Negative flu tests led to COVID-19 testing. Both John and Vicki tested positive. They were sent home to self-isolate. When their symptoms worsened, John and Vicki went to North Kansas City Hospital’s Emergency Department. Vicki was released to go home. John was admitted.
Even then, John wasn’t too worried. Up until he started feeling sick, he was busy with his law practice and stayed physically active by swimming, bike riding or walking at least three times a week. In other words, overall, he was healthy and strong. “I remember thinking I wasn’t that bad,” he said. “I thought I’d be in the hospital a day or so and then go home.”
Touch and Go
John’s condition worsened rapidly. Within just a few hours, he needed a ventilator. “The last thing I remember from that day was being wheeled down the hall to the Intensive Care Unit. It was March 20, 2020.
“Mr. Williams was incredibly ill from arrival,” said Colleen L. Buchinger, MD, one of the many doctors who cared for John. “He required immediate intubation and hemodialysis. He was intubated two different times for respiratory failure and almost needed a third intubation.”
John’s care plan included prone positioning, a therapy reserved for patients with a severe respiratory illness. It involves placing the patient on their stomach to increase oxygen flow to the lungs.
Typically, proning requires a special bed that automatically rotates the patient. In John’s case, the safest option was for his nurses to manually move him.
“I started caring for John on his second day, and I became very invested in his care,” said Emily Layton, an ICU nurse. “His chance of survival was very low, but we never gave up and he never stopped fighting.”
Meanwhile, Vicki was in quarantine at home, battling COVID-19 and worrying about her husband. “I received regular updates, and every doctor I talked to told me John was very ill and may not come out of it,” she shared. “I thought my world would end.”
With the help of the ICU nurses, John’s family, which includes five children and nine grandchildren, set up daily calls. “We told him how much we loved and missed him,” Vicki said. “I prayed every night for God to give his doctors and nurses intellect, compassion and patience. I prayed they wouldn’t give up on him. And, they didn’t.”
John prayed, too. “During my lucid moments, I asked God to forgive my sins and help me,” he recalled. “I had so many people praying for me. That was the big thing. And, I got a lot of help from the doctors, nurses and staff at North Kansas City Hospital.”
While John doesn’t remember the phone calls, he vaguely remembers a FaceTime call with his family, something his nurse, Emily, encouraged his family to try. “After I returned home, I learned they were calling to tell me goodbye,” he shared.
Brighter Days
When the COVID team first took John off the ventilator, he was only able to breathe on his own for about two hours before they had to put him back on it. The team waited another week before trying again.
“It was one of the scariest days,” Vicki said of the second attempt. “I sat in silence and prayer while I waited to hear the result.” The second time was the charm. It was the family’s first sign of hope.
After 33 days in NKCH’s critical care unit, John was well enough to move to the Acute Rehab Unit. His body was extremely weak, and he needed intensive physical, occupational and speech therapy.
“Vicki was John’s biggest cheerleader and advocate,” Dr. Buchinger said. “When John couldn’t speak for himself, she did so loud and clear. When John didn’t feel like participating in therapy, Vicki had a ‘talking to him’ and made sure he did it. She didn’t take no for an answer. I’m positive it made a huge difference that John knew his family was in his corner.”
Prayers Answered
On May 6, 2020, 48 days after he was admitted to the hospital, John was discharged. “I was up at 5 a.m. bugging the nurse to help me shower so I could get ready to go,” he said.
Little did John know a special surprise awaited. Employees who cared for him or who had heard his story lined the hospital hallways to wish him well. “It took my breath away,” he said. “I didn’t know they were going to do that. It was incredible.”
As John recovers at home, he’s looking forward to going out and being active again. “I’m a gregarious person,” he said. “I like to talk and see people and move. I miss going to the movies and eating out. I hope we’ll get back to things we’ve done in the past.”
For now, John’s just thankful. “This disease humbled me more than I’ve ever been,” he said. “It can take anyone down. I thank God for allowing me to survive and be here today. I’m thankful for the excellent treatment the doctors, nurses and staff gave me. And, I’m grateful for the support of my family and friends.”
Related Articles

March 9, 2020
3 Sneaky IBS Triggers
For people with irritable bowel syndrome, spring may spark a flare-up in symptoms

May 31, 2024
5 Nutrition Tips for a Healthier Lifestyle
Healthy eating and proper nutrition play a big part in maintaining good health. Here's how to improve your nutrition habits.
July 8, 2021
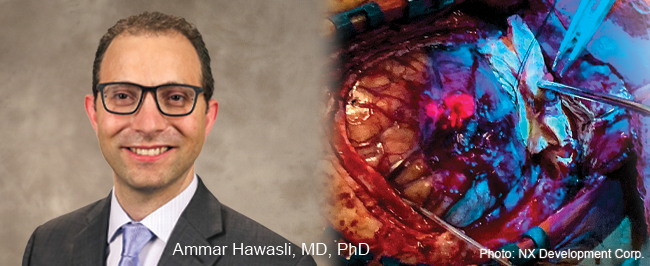
5-ALA Fluorescence Guides Neurosurgeons for More Complete Resections
Neurosurgeons Ammar Hawasli, MD, PhD, and Stephen Reintjes Jr., MD, with Meritas Health Neurosurgery, are now using a progressive treatment that allows for the more precise removal of malignant gliomas and glioblastomas.


