USPSTF Drops CRC Screening Age Five Years for Average Risk People
November 4, 2021Categories: Feature
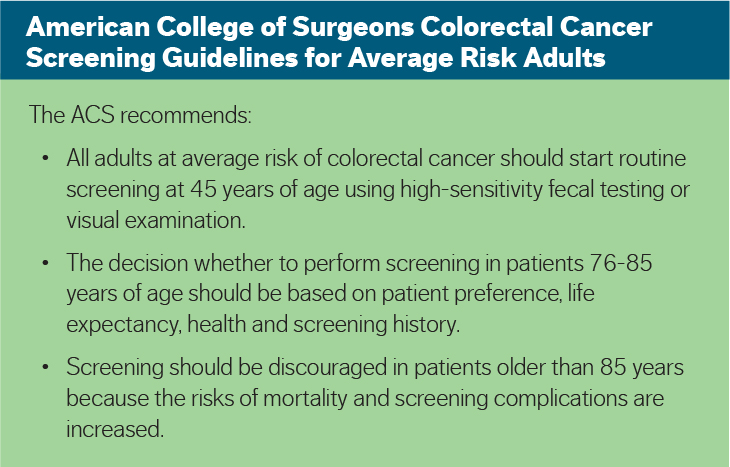
The U.S. Preventive Services Task Force has recommended adults should be routinely screened for colorectal cancer starting at age 45, instead of the current age 50. The rise in CRC cases among young and middle-aged people led to lowering the age.
Although people ages 65-74 comprise the majority of cases, the rates of colorectal cancer diagnosis are on the rise in those under age 50. CRC rates increased every year by 2% in people younger than 50 and 1% in people 50-64 from 2012-2016, according to the American Cancer Society.
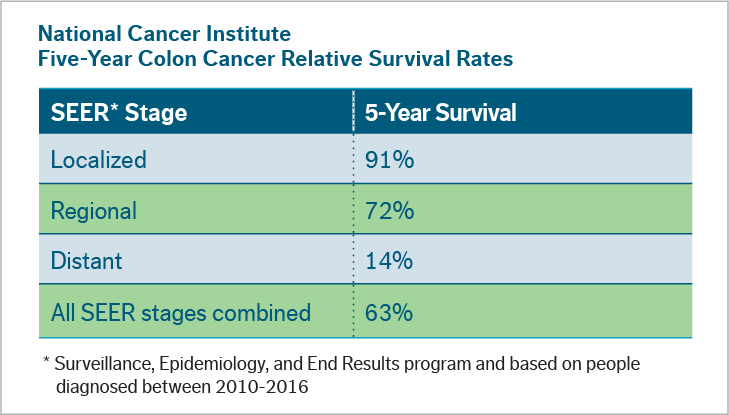
“Screening for colon cancer is the only screening test to prevent cancer,” said James Walden Jr., MD, a gastroenterologist with Gastrointestinal Associated Specialists. “By the time a precancerous polyp becomes big enough to cause obvious symptoms, such as stomach pain, bowel issues and bloody stools, then it’s very likely to be malignant.”
Preventable Disease
The USPSTF found evidence that screening for CRC with stool tests, colonoscopy, CT colonography or flexible sigmoidoscopy in adults ages 45-49 provides a moderate benefit in terms of reducing CRC mortality and increasing life-years gained. The USPSTF rationale summary adds that modeling analyses suggest more life-years are gained and fewer CRC deaths occur when screening begins at age 45 versus age 50.
The ACS reports CRC is the third leading cause of cancer death for men and women, with an estimated 52,980 people in the U.S. projected to die of CRC in 2021. The ACS also noted 10.5% of new CRC cases occurred in people younger than 50 years. Plus, cases among adults 40-49 increased almost 15% from 2000-2002 to 2014-2016.
“We know it takes about 10 years for a polyp to become cancerous so someone who is 50 could have a polyp from before they were 45,” Dr. Walden said. “We want to catch polyps before people develop symptoms. A removed polyp cannot become malignant.”
PCP Recommendation
For Dr. Walden and other gastroenterologists, primary care doctors play a vital role in prevention of progressive disease by recommending CRC screenings to patients at average risk.
“Patients need their physicians to encourage screening, or they will think they don’t need to be screened,” Dr. Walden added.
Some primary care physicians first suggest stool-based methods to screen for CRC, and Dr. Walden agrees with these screening measures.
“Some people are afraid, don’t want to go through a colonoscopy and have seen the option advertised on TV. Doing this type of screening is better than doing nothing,” Dr. Walden said. “However, if their stool-based screening results are positive, the next step is a colonoscopy. And some healthcare insurance companies only reimburse for one CRC screening.”
He advises PCPs to refer their most apprehensive patients to a gastroenterologist, who can further help ease their fears in an office visit. In addition to the ACS guidelines, Dr. Walden pointed to risk factors PCPs should consider from the Centers for Disease Control and Prevention:
- Genetic syndrome, such as familial adenomatous polyposis or hereditary nonpolyposis CRC (Lynch syndrome)
- Inflammatory bowel disease
- Lifestyle factors, including:
- Lack of regular physical activity
- Diet low in fruits and vegetables
- Low-fiber and high-fat diet, or diet high in processed meats
- Excess weight or obesity
- Alcohol consumption
- Tobacco use
- Personal family history of CRC or colorectal polyps

James Walden Jr., MD
Dr. Walden earned his medical degree from Baylor College of Medicine. He completed his residency in internal medicine and fellowship in gastroenterology at the University of Missouri-Kansas City.