Stereotactic Radiosurgery Targets Metastatic Brain Tumors
January 1, 2019A neurosurgeon and a radiation oncologist at NKCH are teaming up to aggressively treat metastatic brain tumors. Their effort centers on advanced imaging and the high-tech guidance of stereotactic radiosurgery, which delivers high doses of radiation to brain lesions while sparing surrounding
healthy tissue.
Using image guidance via NKCH’s Trilogy® linear accelerator, SRS can target multiple lesions (up to 10) as large as 4 cm. Each treatment lasts about 15 minutes. Precision is within 1 mm, with an average 85-90% success rate.
Aggressive Treatment
Historically, people with multiple brain metastases received whole brain radiation when surgery was not feasible or carried excessive morbidity. “Although whole brain radiation therapy is effective, it carries significant cognitive changes afterward,” said Ajay Tejwani, MD, MPH, opens new tab, a radiation oncologist with The University of Kansas Cancer Center. He works full time on the North Kansas City Hospital campus with NKCH’s Radiation Oncology team as part of the hospital’s oncology partnership with The University of Kansas Cancer Center. “With SRS, we can spare normal brain tissue and limit the cognitive side effects. This more aggressive treatment extends disease-free survival and improves quality of life.”
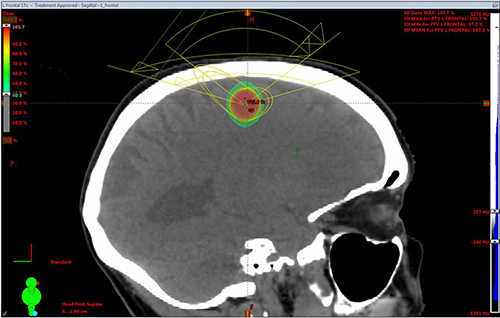
This CT of a patient with metastatic non-small cell lung cancer shows an 8 mm brain metastasis
involving the left frontal cortex, which was treated with a single fraction of radiation.
Stephen L. Reintjes Jr., MD, opens new tab, a neurosurgeon with Meritas Health Neurosurgery, initially evaluates patients to determine if they are surgical candidates. “If their tumor is amenable to resection, it’s typically best for the patient to have SRS after resection,” Dr. Reintjes Jr. said. “If a patient has a brain metastasis, the patient typically will have surgery first, followed by radiation and systemic therapy. Each patient is unique, and we tailor each treatment to the patient.”
Most patients can tolerate SRS. Some experience fatigue, hair loss, mild headache and nausea. There is no anesthesia involved, and patients are custom fitted with a thermoplastic face mask for immobilization. “Afterward, patients are able to return home, while their cancer cells slowly die over the course of two to four weeks,” Dr. Tejwani said.
Some patients are not surgical candidates. Dr. Reintjes pointed to those with metastases of less than 1 cm. They are treated with SRS and then followed with serial MRIs. For lesions precariously located near delicate optic structures or on the brain stem, SRS dosing is fractionated to limit side effects from the radiation.
Both added that beyond brain metastases caused by breast, lung and other primary cancers, SRS is also used on nonmalignant lesions, such as vestibular nerve schwannomas and trigeminal neuralgia.
Collaborative Care
Drs. Reintjes and Tejwani develop SRS treatment plans together. “I know exactly what the tissues look like from performing brain surgery and how they look on the MRI scan postoperatively,” Dr. Reintjes said. “I can then provide guidance for radiating any remaining tumor or the resection cavity.”
Dr. Tejwani, who uses 3D CT imaging to map the targeted area, appreciates Dr. Reintjes’ perspective. “He can identify structures of concern and where a tumor may track,” Dr. Tejwani said. “He provides input, and we collaborate to determine treatment volumes. Having his anatomical expertise is invaluable.”
This collaborative approach is common in centers of excellence. “Many academic centers have this partnership between radiation oncologists and neurosurgeons,” Dr. Tejwani said. “Given the prevalence of patients with brain metastases, it is important providers know they can safely refer them here. I appreciate working closely with our neurosurgeons and its impact on patient care.”
 Stephen L. Reintjes Jr., MD
Stephen L. Reintjes Jr., MD
Dr. Reintjes Jr., opens new tab earned his medical degree from the University of Missouri. During his neurosurgery residency at the University of South Florida, he completed a one-year neurosurgery fellowship in epilepsy at the college and a one-year neurosurgery fellowship at the Swedish Neuroscience Institute.
 Ajay Tejwani, MD
Ajay Tejwani, MD
Dr. Tejwani, opens new tab received his medical degree and master’s degree in public health from Tulane University. He completed a one-year internship at the Tufts University-affiliated Lemuel Shattuck Hospital. He then completed his radiation oncology residency at Weill Cornell’s New York Presbyterian Brooklyn Methodist Hospital.