Health Expert

Sleep. For some, it’s a good night’s sleep. For others, it’s a restless night. Gasping during sleep, daytime sleepiness, loud snoring and morning headaches are just a few of the telltale signs you may be among one in 15 Americans with obstructive sleep apnea.
“Sleep apnea is when you completely or partially stop breathing while asleep, causing oxygen levels to drop,” said NKCH Diagnostic Sleep Center Medical Director Scott Shorten, MD. “This happens when the muscles in the back of the throat fail to keep the airway open.”
This common sleep disorder may also cause:
- Dry mouth
- Frequent nighttime urination
- Memory or concentration difficulties
- Moodiness
- Night sweats
- Sexual dysfunction
Whether you have a few or several symptoms, it’s wise to seek a referral to a sleep specialist, like Dr. Shorten, a neurologist with Meritas Health Neurology.

“Some people are afraid of a sleep apnea diagnosis, but it’s very treatable. Getting good quality sleep can be life-changing,” said Dr. Shorten, who is board certified in neurology and sleep medicine.
He noted that when untreated, sleep apnea can cause other serious health problems, including:
- Congestive heart failure
- Coronary artery disease
- Diabetes
- High blood pressure
- Stroke
Sleep studies are a painless, effective way to diagnose sleep disorders.
At-Home Sleep Study
An at-home sleep study can help determine if sleep apnea is the cause of your sleep troubles. A patient need only wear a band around the chest and two sensors — one on a finger and one under the nose.
After at least seven hours of recorded sleep at home, the patient returns the equipment to NKCH’s Green Hills Diagnostic Sleep Center, where technologists download the data to the patient’s electronic medical record. Patients who have sleep apnea may be treated with a continuous positive airway pressure machine (CPAP) or other alternative, such as a mouthpiece or a surgically implanted mechanism, depending on the severity.
Sleep Center Study
Sleep Apnea Risk Factors
- Age 50 or older
- Body mass index greater than 30
- Cigarette smoker
- High blood pressure
- Neck circumference greater than 17 inches for men and 16 inches for women
Often, when sleep apnea is the diagnosis, the patient will undergo a follow-up sleep study at the sleep center. During the study, a technologist will start a CPAP and slowly increase the settings until the sleep apnea is alleviated. The patient spends a normal sleep period — night or day — in a room with a full-size bed, private bathroom and television.
“A home study is specific to diagnosing sleep apnea,” Dr. Shorten said. “It cannot detect other sleep disorders, such as periodic limb movement disorders. When other diagnoses are suspected or there is a concern for supplemental oxygen or potential seizures, an in-facility sleep study is more appropriate.”
NKCH’s sleep specialists test for more than 20 sleep disorders. Known as registered polysomnographic technologists, they have experience conducting sleep studies tailored to specific needs. They attach special electrodes to the patient’s head, chest and legs. They record when you are asleep and your different stages of sleep. Once asleep, they monitor the patient’s abdomen, chest and leg movement; airflow; brain and eye activity; heart rate and oxygen level. The center is accredited by the American Academy of Sleep Medicine, the leading sleep services accrediting agency.
Sleep and Health
Dr. Shorten’s desire to care for people with sleep issues is rooted in his appreciation of the relationship between sleep and overall health.
“Helping patients carry out their lives in an alert manner so they can accomplish their goals is rewarding,” Dr. Shorten said. “Since I completed my fellowship seven years ago, sleep medicine has continued to gain more recognition as an important foundation for general, physical and mental health.”
ABCs of Sleep Needs
Healthy adults need seven to nine hours of sleep every night — not just over the weekends or as your schedule allows. For some adults, a solid seven hours of sleep may not be enough.
To determine how much sleep you need, ask yourself these questions:
- Am I overly reliant on caffeine to stay alert?
- Do I feel happy and productive the next day?
- Do I feel tired during the day, or am I having trouble concentrating?
Experiment with different regimens within the recommended sleep window to discover what leaves you feeling your best.
Perhaps you know how much sleep you need, but you still have trouble getting it. If that’s the case, try these tips:
- Establish a sleep schedule: Everyone should establish a sleep schedule that ensures they get the proper amount of sleep every night.
- Create a sleep sanctuary: From sheets to room temperature, good sleep relies on the little things. Experts advise leaving the electronics outside of the bedroom to limit your bright or blue light exposure before bed. Keeping the bedroom temperature between 60-67 degrees while you’re sleeping may also help.
- Eliminate disruptions: Despite popular belief, a nightcap can sabotage your sleep. While drinking alcohol may help you fall asleep sooner, it can make it difficult to stay asleep. In some instances, alcohol can exacerbate existing sleep issues like sleep apnea. Drinking caffeine too late in the day may also disrupt your sleep.
Take an online sleep self-test or read more about sleep health at nkch.org/Sleep.
Related Articles

March 8, 2020
3 Sneaky IBS Triggers
For people with irritable bowel syndrome, spring may spark a flare-up in symptoms

May 30, 2024
5 Nutrition Tips for a Healthier Lifestyle
Healthy eating and proper nutrition play a big part in maintaining good health. Here's how to improve your nutrition habits.
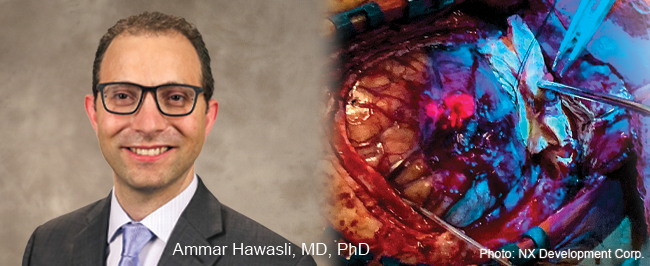
July 7, 2021
5-ALA Fluorescence Guides Neurosurgeons for More Complete Resections
Neurosurgeons Ammar Hawasli, MD, PhD, and Stephen Reintjes Jr., MD, with Meritas Health Neurosurgery, are now using a progressive treatment that allows for the more precise removal of malignant gliomas and glioblastomas.