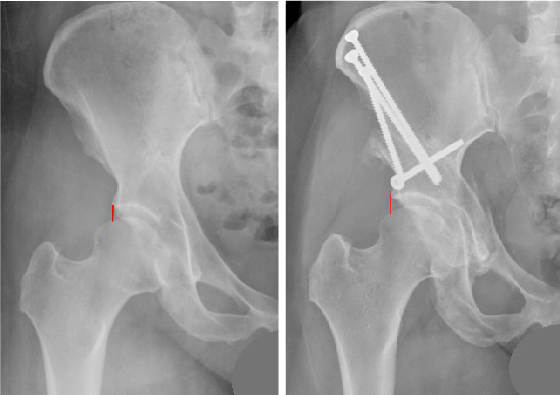
 Images show native hip joint with subtle dysplasia before (left) and after PAO (right). The red lines indicate the acetabulum's edge and femoral head coverage (left), and how the latter increased after surgery (right).
Images show native hip joint with subtle dysplasia before (left) and after PAO (right). The red lines indicate the acetabulum's edge and femoral head coverage (left), and how the latter increased after surgery (right).
Childhood hip dysplasia may not reveal itself until young adulthood, when persistent hip pain causes limited mobility. A malformed socket can cause pain from instability and lead to tears of the cartilage and eventually early onset hip arthritis.
When conservative management fails, North Kansas City Hospital’s Dustin Woyski, DO, performs periacetabular osteotomy, or PAO, to improve function in the hip joint and preserve the natural hip.
“It is not normal for a young patient to have hip pain for any length of time,” said Dr. Woyski, an orthopedic surgeon with Northland Orthopedics & Sports Medicine. “They may have aches and bruises, especially if they are a high school athlete or a physically active young adult, but they need to be evaluated if they have hip pain for more than two to three weeks.”
Difficult Diagnosis
According to the International Hip Dysplasia Institute, adults with hip dysplasia may see more than three healthcare providers and have symptoms for five years before a correct diagnosis is made. Diagnosis is nuanced because the presence of hip dysplasia is subtle.
“Because patients have experienced hip pain and limited mobility for so long, they’ll have had multiple X-rays, MRIs and CT scans. Thus, some or all of their studies can be read as normal, when in fact they have dysplasia,” Dr. Woyski said. “Severe dysplasia may more readily show an incompletely formed socket with the ball completely out of the hip joint, whereas a mildly dysplastic hip may have very subtle findings on imaging studies.”
PAO
Because the hip socket is too shallow to support the ball of the hip and provide adequate stability, Dr. Woyski performs four to five cuts around the acetabulum of the pelvis and shifts it so the head is supported to fit deeper into the hip socket and provide more coverage over the ball. Once repositioned, he places three to four 60 mm-120 mm screws to hold the hip in place so it can slowly heal.
“Repositioning the socket in a more ‘normal’ position over the femoral head prolongs the life of the hip, and there’s good long-term data that supports this,” Dr. Woyski added.
When dysplasia is left untreated, symptoms and joint damage can progress, and patients may require a total joint replacement.
Dr. Woyski considers several factors in determining candidates for PAO, including age and comorbidities, amount of joint deterioration and hip socket displacement, and extent of arthritis.
“An important distinction in considering patients for PAO is the condition of the cartilage. If the cartilage is mostly intact, so with little or no arthritis, then the patient may be a candidate for a PAO,” Dr. Woyski said. “If there is significant arthritis, the only option is a total hip replacement, even in the adolescent child.”
Dr. Woyski’s five- to six-hour surgery, which he performs on a Hana® orthopedic surgery table, combines a PAO with hip arthroscopy to address interarticular issues. The addition of hip arthroscopy is newer and something he learned during fellowship training to address existing hip joint damage, such as labral tears and a coexisting femoroacetabular impingement.
“We have found failures of PAOs are more common in people who have femoroacetabular impingements afterward,” he added. “By correcting their impingements and thus their labral tears when I do
PAOs, we hope their long-term outcomes are better.”
Postoperative Care
After a hospital stay of two to five days, patients are limited to 20-30 pounds of weight-bearing for six to eight weeks. Then they begin another six to eight weeks of physical therapy. Patients will need a walker, shower chair and bedside commode at home, so Dr. Woyski recommends they have a spouse, friend or family member on hand.
“It’s a painful surgery, and they will need assistance for a long time,” Dr. Woyski added.
Patients are discharged with multiple devices to assist with their recovery, including an ice compression machine to reduce swelling and stiffness and a hip brace that attaches to the thigh. Postoperatively, Dr. Woyski sees patients at two weeks, six weeks, three months, six months and one year.
According to the IHDI, 90% of patients report long-term improvements in pain relief and quality of life after recovering from PAO surgery. This includes lasting improvements in sports participation, social life and sex life.

Dustin Woyski, DO
Dr. Woyski earned his medical degree from Kansas City University of Medicine and Biosciences and completed his orthopedic internship and residency at Oklahoma State University/St. Anthony Hospital, Oklahoma City. He was a fellow in hip preservation and reconstruction at Duke University Hospital.