
What is he doing? Marianne Curtis thought. He is just getting a glass of water, then coming upstairs to bed.
Hearing nothing, Marianne went downstairs. There was her husband Scott passed out on the kitchen floor. Marianne ran back upstairs to call 911.
Health Expert

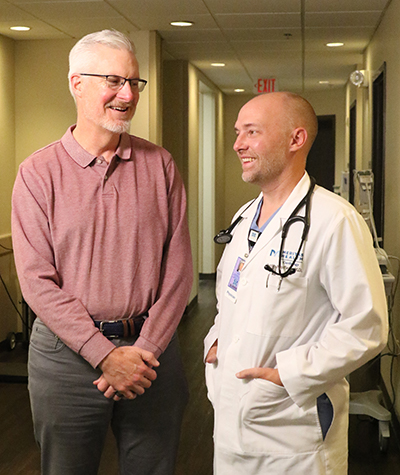
Justin Maxfield, MD
Interventional Cardiologist
Meritas Health Cardiology
816.221.6750
Learn more about
Justin Maxfield.
“I just started doing CPR,” Marianne said. “I ran to open the front door for the ambulance, then went back to CPR. His heart started beating again while I was doing CPR.”
First responders brought Scott to North Kansas City Hospital’s Emergency Department, where staff found an almost total blockage of the left anterior descending (LAD) artery.
The largest artery in the body, the LAD delivers 50% of the heart’s blood supply. As a muscle, the heart needs a steady flow of blood to survive. Despite being an avid runner an a picture of good health, Scott suffered a major heart attack, often called a widowmaker.
“He had a 100% blockage of his LAD that caused him to go into an abnormal and deadly heart rhythm,” said Justin Maxfield, MD, a cardiologist with Meritas Health Cardiology. “The fact that our emergency department, intensive care unit and cath lab team can deal with a critical situation in such a quick manner makes all the difference for the patient’s survival.”
Doctors applied a stent to open the blocked artery. They also put Scott on dialysis to help rid his body of extra fluids and waste while his kidneys were not functioning.
Scott, a science and engineering library liaison at the University of Missouri-Kansas City, recovered. He returned to NKCH three times a week for three months of outpatient cardiac rehabilitation therapy. Treatment here is more than physical exercise. It includes education classes that cover nutrition, mental health and other topics.
Health Expert

Snizhana Weber, CCRP
Exercise Physiologist
Cardiac and Pulmonary Rehabilitation
816.691.1575
Learn more about
Pulmonary Rehab.
“We don’t treat diseases,” said Snizhana Weber, CCRP, exercise physiologist for NKCH’s Cardiac and Pulmonary Rehabilitation services. “We provide education, build stamina, increase strength and help people get back to everyday activities. It’s a holistic approach.”
That approach includes mindfulness and breathing exercises. At the end of each exercise period, patients gather in chairs. The lights go off, relaxing music comes on and patients are asked not to look at their phones or talk.
“It brings patients to the present moment,” Snizhana said. “They don’t have to worry about what is coming next or what happened that brought them to rehab.”
During cardiac rehab, patients are connected to an electrocardiogram (EKG), which records when the heart beats. Snizhana can see heart rates decrease during relaxation and a drop in blood pressure. Patients notice they aren’t as stressed after exercising. There are long-term applications, too.
“We teach these skills so when patients feel anxious, they can dig into these tools and use them,” Snizhana said. “They are always available. You don’t have to remember how to breathe, just remember how to do it properly.”
Scott took these lessons to heart. Before his heart attacks, Marianne said she and her husband were “both high-strung.” They used to absorb and carry the anxiety and stress of life.
Gradually, those parts of Scott changed. He now watches meditation videos on his FitBit app, works with a therapist and has developed a mental toolbox so he can practice mindfulness away from the app. Marianne embraced these changes with him.
“Now we slow down to evaluate the overall situation before acting and reacting,” Marianne said.
Scott still does many of the same things he did before his heart attacks, but his approach is different. Instead of running on a track two or three times a week, he runs on a treadmill. Lifting weights is replaced with resistance band training.
“I use mindfulness to be in the moment,” Scott said. “My heart attack has given me perspective. Not everything is important all the time.”
Because cardiac rehab participants see each other so often, it’s not unusual for them to grow close. “Scott was an example of resilience for his classmates,” Snizhana said.
“Scott has done everything correctly as he recovers,” Dr. Maxfield said. “He knows he has a second chance and he’s taking advantage of it.”
Scott is more practical when thinking about his new chapter in life.
“I will always be grateful to the doctors, nurses and staff at the hospital,” he said.
Mindfulness in Minutes
Practicing mindfulness doesn’t take a lot of time. In fact, you may already be doing some mindfulness exercises without knowing it. The key is putting your mind in the proper space. Here are three easy mindfulness exercises to try.
Make a Gratitude List
Take time each day to reflect on five items you are grateful for and write them down. The goal is to recall an event, person or experience and re-experience the positive emotions.
Mindful Breathing
Focus on each time you inhale and exhale. Clear your thoughts and focus on breathing. You can do this sitting, standing or lying down, with eyes open or closed. Start with five minutes a day and gradually increase the time and frequency.
A Walking Meditation
Mindful walking pays attention to what the body experiences. Start a slow walk. Feel the motion of your feet with each step. Notice how your foot feels both in the air and on the ground. Do this with each step. Gradually expand your focus to sense how your body reacts to each movement. How does the air feel on your skin? What do you see or smell as you move?